Part Seven: The Transplant - 2020
- Caroline King
- Nov 2, 2024
- 12 min read
Updated: Jan 27
18th - 19th May 2020 - QE Birmingham
18th May 2020
Preparing and waiting for the transplant
Once we arrived at the QE again, Jackie wheeled me up to ward 726 gave me a kiss and a hug before wishing me luck. I was on my own again. I had to change into a hospital gown, weight and height taken, the same routine. It was at 5.00 am in the morning. I recall a visit from a lovely surgeon who stopped by to see me, telling me how she wished it was her performing my surgery but was unable to (I can't remember why). Interestingly, she really liked my metal water bottle (how could I remember something as trivial as the water bottle?).
There were two other people on the same ward, one very, very ill lady and a man. That's all I remember. I was determined to stay awake because I thought it might be my last day alive and not survive the surgery. There was no way I was going to sleep. I still had my phone so I was messaging the boys and a few friends with all the strength I had left, hoping I was making sense.
19th May 2020 8.30 am - going down to theatre
Lying on my bed in my gown, semi relaxing with my surgical stockings on, I was thinking that after all these hours, it's going to be another false start. Then suddenly out of the blue two nurses appeared and told me I was going down to theatre. Just like that. I had few minuets to call the boys before my phone was taken away and told that it would be given back to me once I was moved back up to Ward 726 following my time in the critical care unit.
Once again, going down in the lift, it was still eerie and silent being wheeled along the corridors to the theatre. I felt that strange experience again as I did with the Covid test. Although I wasn't panicking at the moment but I do remember when we arrived at the room or pre-med, (it was very loud with lots of clanging noises) panic set in "This is it. I can't believe it's going ahead. I'm actually going to have a transplant, I hope I wake up. I can't leave the boys. I don't want to die". Then blankness.
Extract from the Co-ordinators text to family and friends
Hi all, She made it!
Yeahhhhhhh xxx The consultant said the transfer couldn't have gone any better. The donor liver was perfect and 'slotted ' neatly into place. Finished 2 hours earlier than anticipated due to it going so well!
Days 1-3 in ICU 19th - 22nd May
After the transplant, I recall briefly regaining consciousness in the critical care unit and telling the staff I was very cold. I felt like a tiny creature trembling and need to feel warm. I remember being wrapped in something with warm air being blown into it, and then was heavenly warm and then blackness until I woke up again. Apparently it was some sort of blanket.
A few blinks and say to myself, "I'm alive, I can't believe I'm alive!" Glanced around the room, saw another person to the left of me thinking I wondered what they were here for and then promptly fell back to sleep.
I can tell you from first hand experience, this is no glamorous movie scene with fluttering eyelashes, waking up in full make up, smiling with joy, birds singing and every one in tears, hugging with soppy music playing in the background. This was real time post operation during the lockdown, with no family except the amazing team of surgeons, doctors and nurses.
I fully regained consciousness with medical equipment attached all over me, but I remember the severe pain. The monitors were constantly beeping, and I had a nurse available 24/7. I repeatedly asked for the 'belt' to be loosened because the pain was unbearable. It felt like my stomach was tightened on the last latch of a belt and was about to burst, the pain was intense.
It was clearly the new liver trying to adjust before settling in. This must have been noted as 'an uneventful recovery in CCU for several days'. It was terrible, just terrible. The back pain was terrible and there was a lot of adjustment to make me comfortable. Those initial hours were dreadful, and I drifted in and out of consciousness. Thank you to whoever invented morphine.
I do remember waking up to a bed wash. Afterwards one of the nurses called Tom chatted briefly and he told me that we were the same age and shared the same birthday as he had obviously read my notes. I told him I had a Tom too then fell back to sleep.
Once conscious I had to begin my new medication regimen with water. I have always been good at my water intake, but I struggled to take all the medications with it. I craved something sweet, like squash, which was not available in the CCU but only on the wards. I needed the squash to be able to take the medications, because my body seemed to resist water. I needed some sugar which I explained to the nurse and amazingly, once I had the squash, I could take all the medication without fuss and my energy levels rose.
Still in CCU, I made the decision to go for a walk. It was a challenge to get out of bed and find my balance, but with the help of two nurses on either side, I managed to slowly make my way around the CCU. As we walked, we came to a junction in the ward. If I had turned right, I would have pushed myself too far, so I decided to turn left towards my bed. Once I climbed in, I was immediately sick - it was the water swishing inside me from the medication, but I didn't mention it to the nurses when we were walking. I simply wanted to return to my bed. I couldn't wait to tell Dr. Maltby what I did. I told her I would go for a walk and I did!
While I was awake in the CCU, I often reflected on the generous family who, after losing a loved one, made the selfless decision to donate an organ which allowed me to survive. I experienced such a different arrange of emotions, including the family from the first call. I will always be thankful to my 'donor family' and had already begun mentally what I would say to them in my letter.
May - Moved from ICU to up to Ward 726, Room 23
After spending 3 days in the Critical Care Unit, I was finally transferred to ward 726 and room number 23. I settled in very well, had my phone returned and I finally spoke to the boys. It felt great and apparently I sounded normal again. I also had another water mattress so I was very comfortable and was able to send messages to friends to update them on my condition. I was also given my morphine controlled switch to manage the pain by pressing the button. Whatever they told me to press X amount of times, my mind simply couldn't digest the information and I found myself doing the opposite and pressed it continuously as I felt no pain.
I name the switch 'Fred', god knows why. Anyway, he became my best friend and we settled into a good routine until they took him away after 4 - 5 days. I was horrified and filled with dread as I didn't want to feel any pain again There was no warning, ie, Fred will be with you for 5 days, then he's gone and you're on your own. Why were they taking him away? I'm sure there would have been some tapering down of the dosage and suffice to say, I managed without him by the time of my discharge.
Initially, my recovery was slow, particularly due to the catheter, but once it was removed, I established a routine and began taking small steps forward. The early wake-up call for medication rounds brought back the familiar routine. I found myself faced with numerous medications stored in tiny round white boxes, which took me well over an hour to consume. I asked my nurse about taking some pills after breakfast, but was told to take them before breakfast, especially the anti-rejection ones - either one hour before or two hours after.
Despite my body feeling like an empty shell, I gradually regained my appetite and managed to eat most of the food from the menu.
A few days later, I recall getting up from bed to connect my phone charger. The cable was too short and awkward to charge from the right side. I tried to plug it in from the left side, located behind my chair, so I could charge it on the table next to me. Unfortunately, I miscalculated the distance of the wall plug behind the chair and ended up falling down to the floor, wedged between the chair and the wall, wearing only my hospital gown. I was completely stuck as the chair was heavy and immovable. No one would have known I was there, as any passing nurse would have assumed I was in the bathroom if they glanced through the window.
I realised that not getting up would lead to trouble. I could hear the sound of trolleys being wheeled past and staff chatting, yet I couldn't reach the alarm. Despite trying several times to stand up, my body felt as heavy as lifting a ton of weight (and I was still only tiny). I couldn't tell how much time had passed, but I was growing colder by the minute. It seemed ridiculous that, after finally reaching and having the transplant, I would meet my end due to hypothermia while stuck between a chair and a wall.
Using all my strength, I managed to lift myself up and reach the bed. I climbed in, shivering and rang the bell. Thankfully, they came running. Besides feeling cold and my pride being slightly bruised from attempting to do things on my own, there was no harm done. I did manage to get some extra hospital blankets, though. I eventually recovered, but the experience taught me a valuable lesson. To anyone heading to the hospital, remember to bring an extension lead and make it a long one.
I established another hospital routine and became stronger and coherent with each passing day. It made me realised how very, very ill I was pre transplant. I recall going downstairs for physiotherapy, walking up and down the stairs, and doing other small exercises. Meeting my surgeon during her rounds was just fantastic, and I loved chatting with all the staff. I especially remember a nurse who seemed to think I needed extra feeding, as she would visit me at the end of her shift bringing me stashes of cakes and cheese in case I wanted a midnight snack!
During this time, it was wonderful to reconnect with everyone. I still couldn't believe I was alive and not only that, but I also felt myself growing stronger each day. Catching up with friends through messages and social media was a joy. I could hold a conversation with the boys too. It was great to be able to message again with an almost semi clear head and with eligible messages not gobbledegook which is what I was doing towards the end.
I could also work out Netflix on my iPad. Scrolling through films, most of the new trending ones made no sense to me so I found one that I could relate to. It was like my life had paused in a certain era and I needed to go back to it to relearn how to live again. The Perfect Storm, set in the 90s was the ideal film.
I must have been improving because I recall asking my nurse who the designed the hospital. She had no idea! The messages I received from everyone still amaze me. Of course, I continued to think about my donor family and how they were coping.
The photo below depicts the fall scenario and my food! My chair was positioned to the left of the table, and the plugs for the chargers were located behind the chair.
26th May 2020
Tim and Jackie were invited to the QE to discuss aftercare and medication before being discharged the following day. I recall entering the room with two walking sticks, they were both seated at the far end wearing masks, and I had to stay on the opposite side of the room from them. It was a strange experience seeing family again after the transplant.
27th May - Discharge from QE Birmingham
Extracts from QE discharge letter:
Admitted: 18th May 2020: Ward 726
Discharged: 27th May 2020
Destination: Home
Reason for Admission
• Admitted for potential liver transplant
• Coexisting Medical Conditions
• Chronic back pain (finding)
• Orthotopic liver transplant (procedure)
• Sarcoidosis (disorder)
Procedures
Performed: Procedure: Result: 19.05.2020 Liver transplant Normal
CMV neg to CMV neg
Allergies
Sertraline, Rifampicin, Menthol 1% Aqueous Cream
Medication on Discharge
For precise instructions of when and how to take your medication please refer to the pharmacy label on each drug.
Drug Name Route Form Dose Frequency Duration
0.2% Sodium Hyaluronate
0.2%
Both Eyes Drops (preservative free)
1drop Every Two Hours PRN
To continue
Aciclovir Oral Dispersible Tablet 400mg Five Times a Day (08:00, 12:00, 14:00, 17:00, 22:00)
1 week
Drug Name Route Form Dose Frequency Duration
Adcal D3 Oral Tablet 1tab Twice a Day (08:00, 17:00)
To continue: Adoport (BD Tacrolimus) Oral Capsule 3mg Twice a Day (10:00, 22:00)
To continue: Alendronic Acid Oral Tablet 70mg Once a Week [Wed] (08:00)
To continue: Aspirin Oral Dispersible Tablet 75mg Once a Day (22:00)
To continue: Co-trimoxazole Oral Tablet 480mg Every Other Day (08:00)
To continue: Dorzolamide/ Timolol (Cosopt) Both Eyes Drops 1drop Twice a Day (08:00, 17:00)
To continue; Lansoprazole Oral Capsule 30mg Once a Day (06:00)
To continue: Latanoprost Both Eyes Drops 1drop Once a Day (22:00)
To continue: Laxido ( macrogol ) Oral Powder 1Sachet Twice a Day (08:00, 17:00)
2 weeks Meritene Energis Shake Oral Powder 1Sachet Three Times a Day (08:00, 12:00, 22:00)
To continue: Morphine Sulfate Oral Solution (10mg/5ml)
Oral Oral Solution 5-10mg Every Four Hours PRN 1 week
Morphine Sulfate Sustained Release Oral Capsule 90mg Twice a Day (10:00, 22:00)
To continue: Mycophenolate Mofetil Oral Tablet 1g Twice a Day (10:00, 22:00)
To continue: Nystatin Oral Suspension 200000units Four Times a Day (08:00, 12:00, 17:00, 22:00)
To continue: Prednisolone (Not enteric coated) Oral Tablet 20mg Once a Day (06:00)
To continue: Renapro Shot Oral Liquid 60ml Three Times a Day (06:00, 14:00, 22:00)
To continue: Senna (Sennosides) Oral Liquid 10ml Twice a Day (12:00, 22:00)
To continue: Xailin Night Eye Ointment Both Eyes Eye ointment 1Application Once a Day (22:00)
Discharge Notes
This 57 year old lady was admitted to QEHB Liver Unit on 18/5 for Liver Transplant for Hepatic Sarcoid. On admission she was well and had a CT thorax which showed no signs of Covid infection.
Background:
Ductopenic Granulomatous Hepatitis secondary to systemic sarcoidosis
Cushingoid secondary to long-term steroids
Osteoporosis - multiple spinal fractures
Severe Glaucoma - operation 24th March 2020
Chronic back pain
Admission details
On 19/05 the patient underwent a DBD CMV -/- modified piggyback liver transplant. Post operatively she had an uneventful recovery on the ICU for several days. Her pain was managed with a PCA and then this was stepped down to oral analgesia. On 22/5 she was stepped down to ward 726 where she continued to improve. There was a small amount of abdominal fat protruding from one of her drain sites, this has been
manually reduced and sutured and has not caused further issues. She has continued to improve clinically and is now medically stable for discharge.
Information Given to Patient
Please seek medical attention if you are feeling unwell
After Hospital admission, you are at increased risk of blood clots (thrombosis). For further
information about the symptoms of Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE) and what you can do to reduce your risk, please see the video and information leaflets on our website (https://www.uhb.nhs.uk/dvt)
Recommendations for GP
Please note medication changes detailed above. Please remove drain site stitches 7th June.
Please inform AnticoagulantTeam@uhb.nhs.uk if this patient develops a deep vein thrombosis or
pulmonary embolism within 90 days of discharge.
Risk of falls: The latest Falls assessment suggests that the patient is at risk of falls.
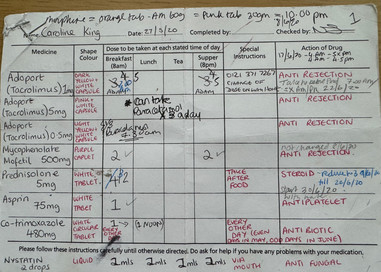
On the day I was discharged, I received my list of medications. My nurse tried to patiently explain them all, but I found it overwhelming and couldn't take all the information, including her instructions. These were the same medications I had been taking daily, but the nurses had administered them in succession, one by one, in small white paper bowls. It was a simple process then, but now I had to manage it independently. This is going to be a total nightmare I remember thinking when I get home. I'm going to get confused and muddled. I had to take one step at a time.
12 June 2020 - RUH
Extracts from RUH letter:
I called Caroline for a planned telephone consultation today and was absolutely delighted to see a letter from the Birmingham team which we received on the 9th June showing that a liver transplant went ahead for her in mid-May. Unfortunately, Caroline wasn't able to take the call this afternoon, I wonder whether she might be up in Birmingham at a further follow-up appointment. At this stage she was seen in Birmingham on the 1st June. She was progressing well and satisfactory blood tests and a plan was made for gradual reduction of her opioid analgesia. Interestingly, I note that the ex-planted liver did not show significant granulomatous change which might be against the initial diagnosis of Sarcoidosis. This diagnosis was made on the basis of a liver biopsy performed in May 2019 which showed multiple non-caseating granulomas in the context of also having unexplained recurrent Uveitis. I wonder whether it is possible that her liver histology may have been modified by her steroid treatment. I note that she has been commenced on Ursodeoxcholic acid because of the possibility of an alternative diagnosis of antibody negative PCB. I really hope that Caroline continues to progress well. In the immediate period post-transplant she will be under quite intensive follow-up by the team in Birmingham so for the time I have not planned a further follow-up appointment with her for 2 months. However, I would be very happy to check in with Caroline by telephone should anything be needed. I have subsequently spoken to Caroline on the telephone the following day and was pleased to hear her feeling so much better and more positive. If it facilitates communication about Caroline's care, my secretary's details will be at the bottom of this letter if the Birmingham team should wish to email the letters rather than sending them in the post.
Told Dr Maltby about my walk around CCU.















Comments